Warning!
New Zealand has several IVIG products. Each has different rates for administration. Please check you have the correct infusion rate for the specific IVIg product you are administering.
Presentation
- 5g (50mL), 10g (100mL) or 20g (200mL) bottles
- Privigen is a 10% solution of human immunoglobulin(antibodies) (10g/100mL) prepared from pooled plasma donations made from European and North American donors for intravenous use.
- For subcutaneous immunoglobulin, please see the dedicated pages.
- For a list of all immunoglobulin products, please see here.
Infusion calculator

Australian NBA IVIG Guideline

English NHS IVIG Guideline

Fluid chart for Privigen
Prescription
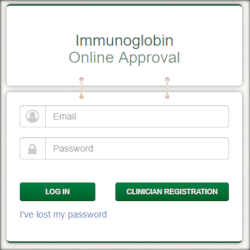
- Because Privigen is an expensive medication with increasing demand, pre-approval of new patients receiving intravenous immunoglobulin is required. Please see the guidelines provided on the right and use on the online approval tool or complete the pre-approval form, also on the right. If urgent, please contact the Transfusion Medicine Specialist on call.
ABO Compatibility
- Compatibility is not relevant for manufactured (fractionated) plasma product transfusion, however see Precautions below for risk of haemolysis in group A patients.
Storage and Infusion
- Infuse once the bottles have reached room temperature. If there is a delay, return to Blood Bank, or store at 2-8°C in a blood bank approved vaccine or blood refrigerator. Do not refrigerate after the bottles have reached room temperature.
- During storage protect the bottles from light.
- Multiple bottles of the same batch may be pooled together.
- Do not shake the bottles (causes frothing).
- Use a vented infusion set or a standard infusion set with a venting spike. Spike the bottle stopper in the centre to minimise stopper dislodgement.
- A blood filter is not needed.
- If not used, please return to Blood Bank promptly.
Precautions
- Hydration: Ensure your patient is adequately hydrated as patients with pre-existing renal impairement, diabetes mellitus, volume depletion, sepsis, paraproteinaemia, or those taking concomitant nephrotoxic drugs or who are more than 65 years old are at risk of acute renal failure. Renal function should be monitored in these patients.
- Patients with Group A red cells should be monitored for haemolysis (see manufacturer's instructions) as Privigen contains anti-A and anti-B antibodies.
- Passive Transfer of Antibodies and Interference with Serological Testing: After injection of immunoglobulin, the transitory rise of the various passively transferred antibodies in the patient's blood may result in misleading positive results in serological testing.
- Read manufacturer's instructions carefully
- Always observe for turbidity, floating material and sediment
Vaccinations
- Inactivated vaccines (e.g. flu, hepatitis B, tetanus, pneumococcal): Inactivated vaccines may be administered concurrently with passive antibody to induce active immunity.
- Live attenuated virus vaccines (e.g. meales, mumps, polio, rubella): Passively acquired antibody can interfere with the response to live, attenuated virus vaccines. Administration of such vaccines should be deferred until approximately three months after passive immunisation. If immunoglobulin is administered within two weeks of vaccination with a live attenuated virus vaccine, the efficacy of the vaccine may be compromised. Consideration should be given to re-vaccination approximately three months after the immunoglobulin was given.
Rate
- Privigen contains no preservatives to prevent bacterial growth so each bottle should be infused within 4 hours of spiking
- The first infusion should be administered at an initial rate of 0.3 mL/kg/hour.
- If the infusion is well tolerated, the rate can be doubled at 30 min intervals to a maximum rate of 2.4mL/kg/hour, at the discretion of the healthcare professional and as tolerated by the patient.
- For subsequent infusions a similar step-wise approach can be used, as tolerated. i.e. commence at 0.3mL/kg/hour, increasing the rate every 30 minutes, as above.
- For regular recipients (e.g. PID, secondary hypogammaglobulinaemia, CIDP): from the fourth infusion onwards, the maximum infusion rate (as tolerated) is 4.8 mL/kg/hour.
- Rates are discussed in detail in the CSL Behring's Privigen infusion guide.
- In patients at risk for acute renal failure, thromboembolic adverse reactions, IVIg products should be administered at the minimum rate of infusion and dose practicable.
- Slower infusion rates will diminish rate related symptoms such as headache, shivering, tachycardia and BP alterations.
- Electromechanical pumps are recommended for infusion.
- There is no need to slow the infusion down if changing between bottles of different batch numbers of Privigen.
- In order to finish each bottle in 4 hours or less,
- children under 15 kg should only receive the 5g bottle size.
- children weighing 15-30 kg should only receive 5g or 10g bottle sizes.
- children and adults weighing 30kg or more can receive 5g, 10g or 20g bottle sizes.
- NOTE when using Guardrails: when programming the pump with the infusion rates calculated above, you may get a "maximum rate exceeded" alarm. In that situation we advise that you run the infusion at the maximum rate that the pump profile allows.
Monitoring
- Reactions tend to be related to the infusion rate (i.e. faster rate = more severe reaction) and are most likely to occur during the first hour of the infusion.
- It is recommended that the patient's vital signs and general status are monitored regularly throughout the infusion.
- It is recommended that the patient's temperature, pulse, BP and respiratory rate are monitored:
- every 15 minutes for the first hour
- twice in the next hour
- and hourly for the duration of the infusion
- Monitoring should also include urine output and serum creatinine.
- There is no change in monitoring between bottles
- For patients who are naïve to human Ig, switched from other Ig, or who have had a long interval since previous Ig infusion, monitor for an hour post infusion. All other patients only need to be monitored for 20 minutes post infusion.
- In case of an an adverse reaction, the rate of administration must be reduced or infusion stopped. The treatment required depends on the nature and severity of side effect.
- Report all adverse events to Blood Bank – contact your local transfusion medicine specialist or transfusion nurse specialist for advice.
DO NOT
- DO NOT add medications to blood products.
Dose
- Replacement therapy (for immunodeficiency): adjusted for the individual patient. Typically 0.2 - 0.8 grams Privigen per kg bodyweight per month. Higher doses may be needed initially following diagnosis (0.4-0.8 g/kg).
- Immunomodulatory therapy
- ITP: optimal dose determined for each patient. Up to 2 grams Privigen per kg bodyweight divided over 2-5 days.
- Guillain Barre Syndrome: 0.4 grams Privigen per kg bodyweight per day over 5 days.
- Kawasaki's Disease: 1.6 - 2 grams Privigen per kg bodyweight divided over 2-5 days or 2 grams per kg as a single dose.
- CIDP: initially 2 g/kg over 2-5 days then 1g/kg every three weeks over 1-2 days
- Multifocal motor neuropathy: initially 2 g/kg over 2-5 days then 0.4-2g/kg every 2-6 weeks
- Myasthenia gravis: induction, prior to surgery or during a crisis: 1-2 g/kg over 2-5 days then 0.4-1g/kg every 4-6 weeks
- Lambert-Eaton myasthenic syndrome: induction: 2 g/kg over 2-5 days then 0.4-1g/kg every 2-6 weeks
- Stiff person syndrome: induction: 2 g/kg over 2-5 days then 1-2g/kg every 4-6 weeks
- Treatment / prophylaxis of specific infections: please see this document
More Info
- Information on Changes to New Zealand's Immunoglobulin products
- Timelines for roll-out of IVIG changes
- Privigen vs PrivigenNZ
- Patient Information brochure
- Patient Information Leaflet
- Product Overview and Infusion Guide (CSL Behring)
- Datasheet
- Consumer Medicine Information
- Transfusion Medicine Handbook
- NZBS Immunoglobulin Hub
- Ig Hub - Privigen
- NZBS Clinical Compendium